If you've ever had a cold sore, you likely have herpes — and that's OK! Herpes is super common (you may have it and not even know it!). It’s nothing to be ashamed of.
While there's no cure for herpes, there are ways you can protect yourself and your partners from contracting or spreading this misunderstood (and often stigmatized) virus.
Here's everything you need to know about herpes, including how it's spread, what symptoms to look out for, and what you can do to manage it.
What is herpes?
Herpes is a common, incurable sexually transmitted infection (STI) caused by the herpes simplex virus type 1 or type 2 (HSV-1 or HSV-2). According to John Hopkins Medicine, 50-80% of adults have HSV-1, which can cause cold sores or blisters in or around a person's mouth or genital areas. Genital herpes (caused by HSV-1 or HSV-2) affects one out of six Americans aged 14 to 49.

How do you get herpes?
Herpes (either HSV-1 or HSV-2) is contagious and is spread by direct contact with a herpes sore, or from an infected person's saliva, genital secretions, or blood while the virus is still shedding. Herpes is most likely to spread during an outbreak. However, the virus can be transmitted even when the carrier is asymptomatic (meaning they don't have an active herpes sore, aka cold sore).
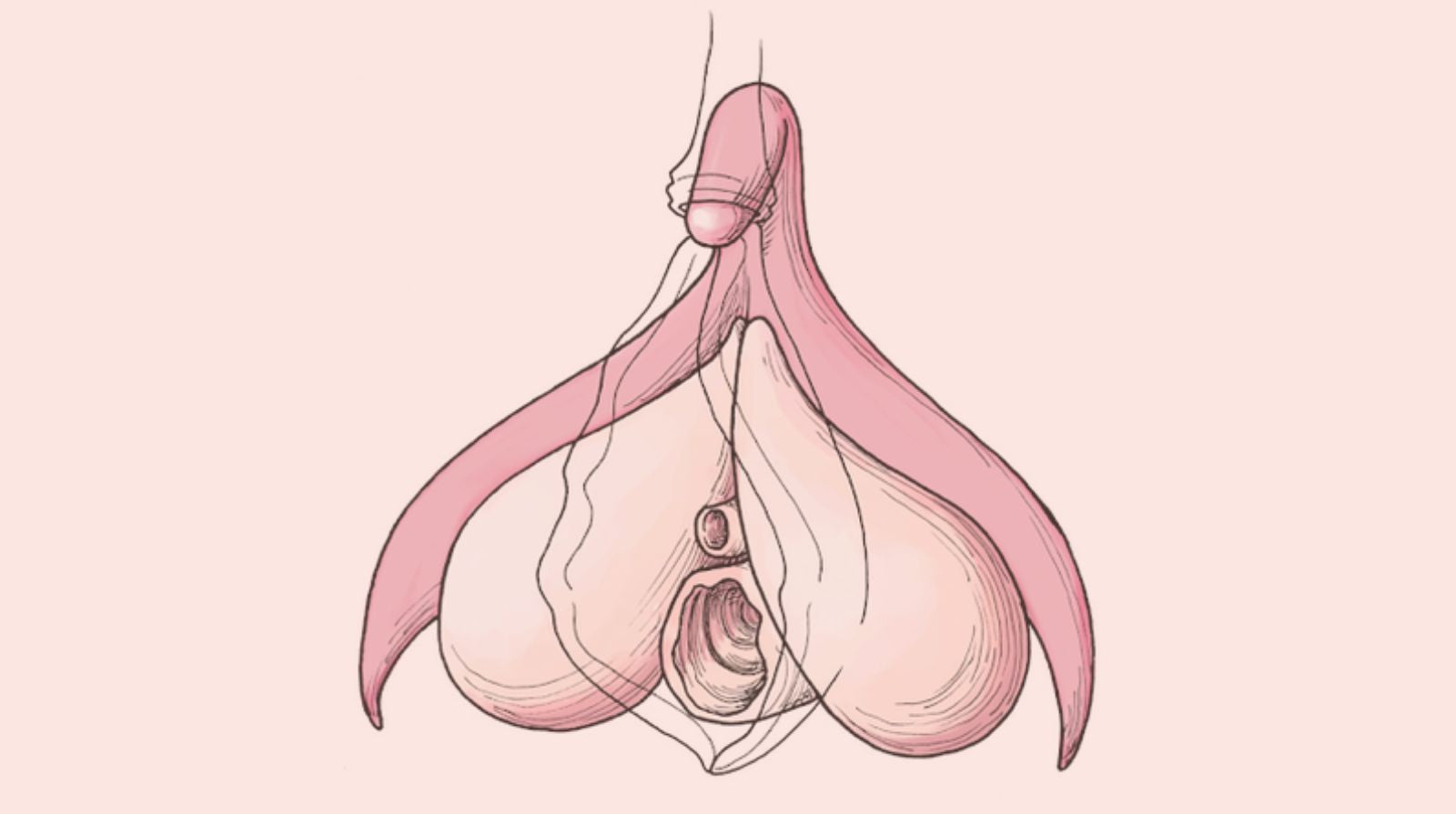
Anyone can get herpes. Even if you and/or your partner are wearing a condom, you can still contract the virus. This is because the condom only protects the area it covers! So, the pelvic area, mons pubis, labia, the base of the penis, and the mouth and tongue are at risk.
"Herpes is most contagious when the sores are open and 'wet,'" says Amir Marashi, OB-GYN, and CEO of CERĒ. "It's spread from skin-to-skin contact with someone who has the virus and is commonly spread through oral, anal, and vaginal intercourse." And yes, herpes can also be tranmitted through rimming or anilingus.
In 2019, Weil Cornell Medical School researchers discovered that HSV-1 (oral and genital) might be more transmissible during oral sex than intercourse. Approximately 90% of new genital herpes cases are HSV-1 from oral sex.
HSV-1 vs. HSV-2
The herpes simplex virus is divided into two types: HSV-1 and HSV-2. Both kinds of herpes can appear on the lips, mouth, throat, eyes, vulva, vagina, cervix, penis, scrotum, inner thighs, butt, and anus.
Oral herpes
If you have HSV-1 or HSV-2 in the oral area (lips, mouth, throat), it's called oral herpes. (This includes cold sores, but we'll get to that in a minute.)
Possible symptoms of oral herpes:
- swollen gums
- swollen neck lymph nodes
- painful, fluid-filled blisters on or in and around the mouth (typically on the edges of the lips)
- fever
- muscle aches
- headache
Yes, cold sores are herpes too!
Cold sores are just another name for herpes sores, and are caused by the herpes simplex virus. According to Dr. Marashi, many people with oral herpes acquire it during childhood (e.g., being kissed by a parent with a cold sore).
"Touching someone’s herpes sore and then touching your eyes or mouth (without washing your hands) is another common way to acquire herpes," adds Dr. Marashi. "The virus can also enter the body through an opening in the skin, such as a rash, burn, or other sore. The good news is, you can’t get herpes by holding hands, hugging, coughing, sneezing, or toilet seats."
Genital herpes
If you have HSV-1 or HSV-2 in the genital area (vulva, vagina, cervix, penis, scrotum, inner thighs, butt, and anus), it's called genital herpes.
Possible symptoms of genital herpes:
- painful, fluid-filled blisters on or around the genitals (typically on the genitals, anus, and inner thighs)
- itching
- swollen glands
- fever
- chills
- headache
- body aches
- fatigue
"When herpes is caused by HSV-2, flu-like symptoms can occur, including fever, chills, swollen lymph nodes, headache, generalized body aches, and fatigue," says Dr. Marashi. "The first herpes outbreak is generally the most painful and lasts two to four weeks. The blisters and sores resolve, but the virus remains in the body, making future outbreaks possible," Dr. Marashi continues. "Itching and burning sensations in the affected area can be a sign that another outbreak is about to occur."
Diagnosis
"The only way to know what type of herpes you have is through a test," Dr. Marashi tells Lorals. "If there's a herpes outbreak, a doctor can take a sample of the blister or sore and send it for testing. Performing a blood test for HSV-1 and HSV-2 is another option."

Unfortunately, getting an accurate blood test result is difficult and false positives are common. According to the Centers for Disease Control and Prevention (CDC), the chance of receiving a false positive herpes test result is much higher than when testing for other STIs, such as gonorrhea and chlamydia. If you get a blood test too soon, the results could be wrong.
Herpes blood tests have a sensitivity level of 80–98%. Because herpes serologic tests detect antibodies of the herpes virus (and not the virus itself), there’s a possibility the results will be inaccurate depending on when the test was taken. For example, if you’re tested too soon (>48 hours) after becoming infected, you may receive a false negative.
Additionally, herpes serologic tests are unable to distinguish between HSV-1 and HSV-2 antibodies. The only way to learn whether you have HSV-1 or HSV-2 is through a swab of an active sore.
The CDC doesn't recommend herpes testing (by blood test or swab) for people who have never had a herpes outbreak, as the chances of receiving inaccurate results are higher for people at low risk of infection. And most medical providers do not include it on a standard STI panel, so you would have to request it explicitly.
A blood test may be helpful for people who:
- have genital symptoms that could be herpes-related
- have (or had) a partner with genital herpes
- are experiencing or noticing signs of herpes
Treatment Options
Once you get herpes, you have it for life. That said, treatment options can help you manage symptoms and reduce the likelihood of future outbreaks.

Some treatment and pain management options for both oral and genital herpes include:
- oral antiviral medications (e.g., Valtrex or Sitavig)
- topical antiviral ointment (e.g., Zovirax)
- over the counter ointment (e,g., Docosanol)
- over-the-counter pain relievers (e.g., acetaminophen or naproxen)
- aloe vera gel or petroleum jelly
- creams and/or lotions (e.g., benzocaine)
You can also ease the pain with warm baths or showers, keeping the affected area dry (moisture prolongs the duration of the blisters and sores), wearing loose clothing, and applying an ice pack (covered or wrapped in a cloth) to the area.
"If you have an outbreak, try not to touch the sores, since this can spread the infection to other parts of your body, and to other people," says Dr. Marashi. "When you touch the sores, be sure to wash your hands with soap and water."
How to Get Rid of Cold Sores Inside Your Mouth
Most cold sores heal within seven to 10 days. Waiting for a cold sore (especially one that’s on the inside of your mouth) to heal on its own, however, may be uncomfortable or painful.

To help speed things up, you can purchase an antiviral cream or cold sore patch (that contains hydrocolloid gel) online or at your local pharmacy.
You can also schedule an appointment with your dentist — they’ll be able to help you identify whether your sore is a cold sore or a canker sore, prescribe an antiviral medication, and/or perform laser therapy.
Protecting Yourself and Your Partner
If you have herpes, it's important to tell your partner (or partners) to take proper precautions.

You can prevent the spread by:
- using a condom or other barrier method (like Lorals!) during oral, anal, and vaginal sex
- being open and honest with your doctor and your partners
- avoiding sex during a herpes outbreak
- avoiding sharing drinks and utensils if someone is experiencing an outbreak or symptoms
- getting tested regularly for STIs (herpes is not on a standard panel)
- taking antivirals to prevent or shorten outbreaks
How do I protect against herpes during oral sex?
While the main focus of STI protection tends to be condoms, the reality is that most people are having way more sex that doesn't involve the penis – like cunnilingus and rimming – so condoms won't really help with that. Using barriers during oral sex, like dental dams or Lorals, helps to protect you. Lorals are ultra-thin latex undies you wear during oral-vaginal sex and oral-anal sex, and yes they do protect against herpes. Why wear Lorals during oral?
- Lorals cover more! They come in Bikini and Shortie styles with full coverage of the genitals and anus, so your partner gets full access and you both get the protection you need.
- Lorals are designed to stay in place. Unlike dental dams, they're wearable and hands-free, so you and your partner can use your hands for more pleasurable activities.
- Lorals are SEXY! They adapt to your body so they can fit like silky lingerie or your favorite comfy undies. Bonus: They’re great for role-playing.
The Bottom Line
Herpes is contagious, but that doesn't mean you can't have sex or be intimate with your partner or future partners down the road.
According to Herpes Opportunity, women with genital HSV (who are not having an active outbreak) have a 4% risk of transmitting the virus to their partner during intercourse. Men have a 10% risk of transmitting to a woman. (Condoms cut this risk in half!) Additional research suggests that daily antiviral therapy can cut your risk in half again — 1%, and ~2%, respectively.
“HSV-2 is mostly transmitted through vaginal or anal intercourse,” says Dr. Marashi. “It’s rarely transmitted through oral sex. However, HSV-1 is more transmissible than HSV-2 through oral sex.”
Being diagnosed with herpes isn’t the end of the world. Herpes is super common and typically asymptomatic in most people. And, once you receive a positive diagnosis you can work towards having a mature and fulfilling sex life in which you and your partners communicate clearly about your health issues, risks, and fears – just like every other healthy relationship, herpes or not.
Written by Tabitha Britt, a freelance writer and editor. She's also the founding-editor-in-chief of DO YOU ENDO, the first (and only) no-BS digital magazine for individuals with endometriosis by individuals with endometriosis in the US. You can find her byline in a variety of publications including Insider, Medical News Today, and Kinkly.
Reviewed and Edited by Sarah Brown, a sex and intimacy educator with 10 years of experience designing and marketing intimate wellness and pleasure products.